Ebola & HIV with Many Dangerous Unknowns: Impact of U.S. Foreign Aid Cuts
Among the confusion generated by the Trump administration’s funding cuts, restarts, terminations, waivers, layoffs, and overall lack of communication about the reduction in U.S. foreign aid, we are all left with much less information about the epidemics that impact everyone.
Ebola outbreak with so many questions
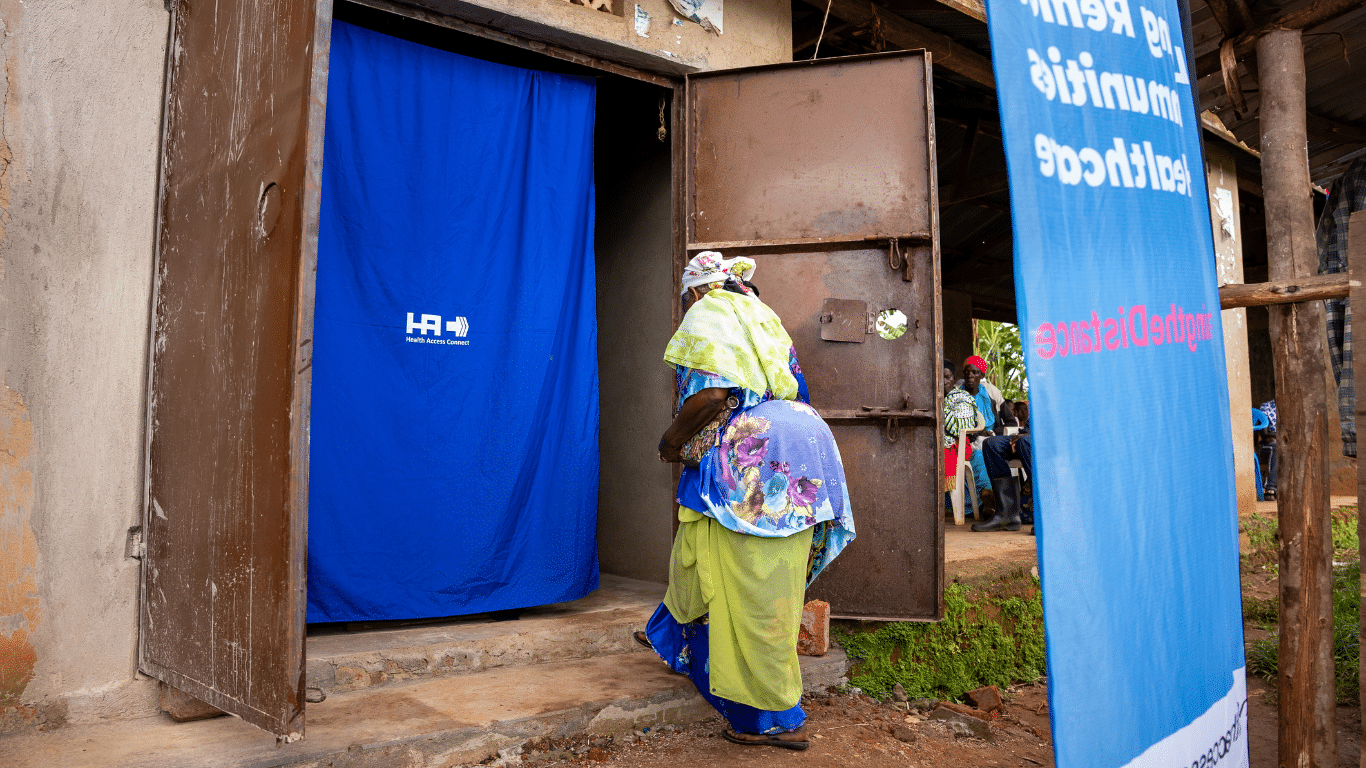
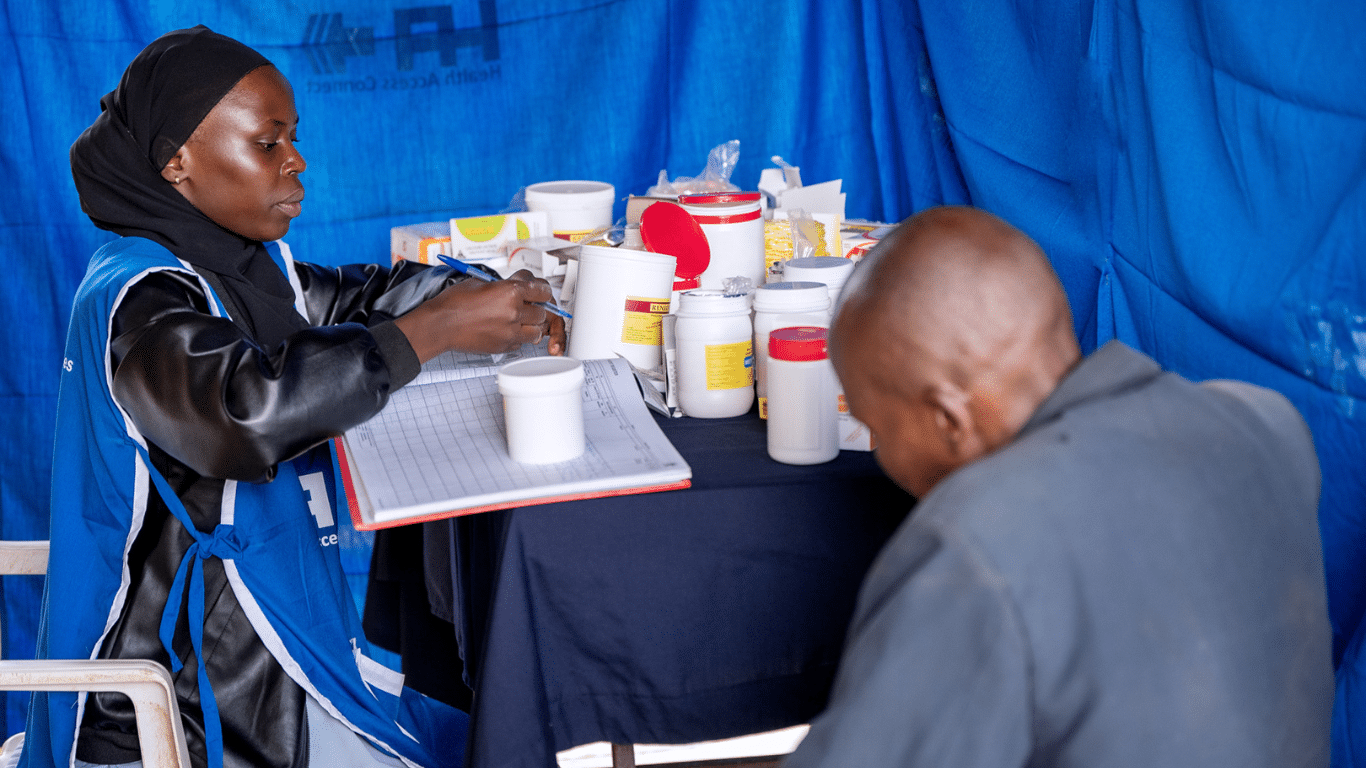
Uganda has seen outbreaks of Ebola and other diseases multiple times in the recent past. The Ugandan Ministry of Health has worked closely with partners from the World Health Organization, as well as U.S. organizations, including the Centers for Disease Control and Prevention (CDC) and the U.S. Agency for International Development (USAID), to help assess and contain outbreaks. They have provided support in knowledge, equipment, medicine, and funding.
During an Ebola outbreak in Uganda this year, all US Ebola response funding was cut and then supposedly restarted. However, the conditions of the funding restart are not clear. Reporters have reached out to me for answers since I work in public health in Uganda. But I don’t work directly in outbreak response, so I can’t really help with reliable information. Reporters have told me that when they approach American or Ugandan government representatives, they have been unwilling to share information on exactly what is going on.
The result, effectively, is that we do not really know what the status of the Ebola outbreak is. Has it been contained? Does the Ugandan government need more support? Where are the dangers in the country? Has the disease spread beyond borders?
I have spoken with several people who work in disease response, and they have told me that healthcare workers are participating in the response without pay. They have no idea what support they might ultimately receive. Employees of USAID who had the ability to move funds, procure equipment, and assist in the coordination of the response have been laid off or placed on administrative leave.
HIV without a clear way forward
There are about 1.5 million people living with HIV in Uganda right now. Since 2003, the U.S. government has worked in close collaboration with the ministries of health around the globe to help distribute medicine and provide health services to people living with HIV. These investments were suspended or cut entirely in the first wave of communications from the U.S. Department of Government Efficiency (DOGE). Some were then restarted under uncertain terms.
The global HIV response depends on billions of dollars being allocated in multi-million-dollar grants to governments, international bodies, and public health organizations around the world. These grants are implemented by people with specialized skills. Service providers are supported by robust organizations that have been designed around serving people, reducing infections, and moving toward eradicating the disease. Funding has resumed for much of this response, but there have been major gaps and confusion. The people I know who work at these organizations say that they have had to cut many critical staff members, and they are dealing with a lot of uncertainty introduced by reporting to people who are not familiar with their work. That includes being constantly asked to submit new plans, justifications, and realignment strategies over and over. Those demands mean that highly skilled people are unable to use their limited time to actually fight HIV.
Uncertainty is dangerous
If healthcare providers don’t know if they will have medicine, equipment, and support, we cannot expect them to conduct the critical and often dangerous tasks our societies depend on them to do. The cuts to U.S. foreign aid have been abrupt, naive, poorly planned, poorly communicated, and dangerous. Many lives are at risk RIGHT NOW (as many as 25 million in one estimation) if we are unable to coordinate a unified approach to some of the most lethal diseases and necessary health services.
We need to fight for the return of U.S. foreign assistance
The U.S. investments to reduce poverty and inequality in the world are some of the best uses of our tax dollars. As someone who has spent his career in international development, I can think of many ways that U.S. foreign assistance could have been approved. As a patriotic American, I am so proud of the causes we have supported, the lives we have saved, and the lives we have improved. We must fight for that.